The Brain on Stress: A Neuroscience Primer
The Brain on Stress: A Neuroscience Primer
Human brains under stress do all kinds of strange, frustrating, and completely explainable things. Understanding how stress works in the brain has made an impactful difference for me in how I see myself, my old burnout patterns, and the people I support.
So here’s a (hopefully) gentle, science-based primer on what’s actually happening in your body and brain when stress takes over, and how we can begin to live in relationship with stress.
Meet Your Stress Brain: The HPA Axis, Amygdala & Prefrontal Cortex
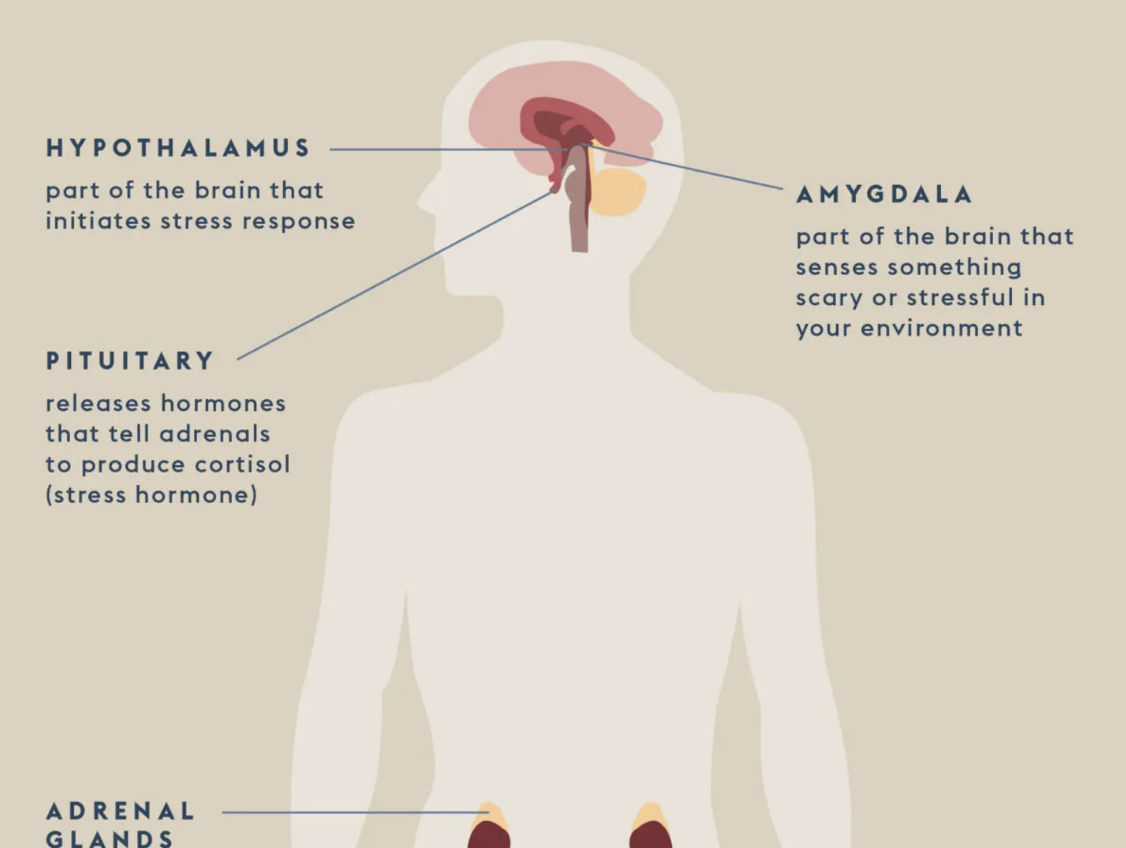
Let’s start with the biology basics. When we talk about stress in the body, we’re usually referring to the activation of the HPA axis — a system made up of the hypothalamus, pituitary gland, and adrenal glands. This trio works together like a high-alert communication chain. The moment your brain senses a threat (real or perceived), this system kicks into gear, pumping out cortisol and adrenaline to help you deal with the danger.
The amygdala is often the one sounding the alarm. It scans constantly for anything that feels unsafe — which may actually be something like conflict, rejection, deadlines, or even a tone of voice that reminds you of something painful. When the amygdala is triggered, it sends a message to the HPA axis: Sound the alarm! The heart races. Muscles tense. Your breathing gets rapid. You get tunnel vision. You’re now in survival mode.
At the same time, your prefrontal cortex — the part of your brain responsible for problem-solving, emotional regulation, and executive function — goes offline. It’s not that you’ve forgotten how to cope. It’s that your brain is prioritizing immediate survival over nuanced reflection. This is brilliant, evolutionary design and thank goodness for it! But in our modern lives, where the threat is a performance review or a packed schedule, this system gets taken over a lot.
Chronic Stress Changes the Brain
Here’s where it gets tricky. Our stress system was built for short bursts: get to safety, then calm down. But many of us live in a state of chronic stress. Deadlines pile up. Slack messages ping us constantly. Care responsibilities seem to never pause. And for those navigating systemic oppression, financial insecurity, or intergenerational trauma, that stress can feel all consuming and endless.
Over time, chronic stress can shrink the prefrontal cortex, enlarge the amygdala, and impair memory and concentration. It can dysregulate our sleep, digestion, hormones, and immune responses. It doesn’t just feel hard — it is hard, on a neurological level. But your brain is not failing. It’s adapting.
Trauma and the Nervous System
When stress overwhelms your ability to cope or make meaning, it changes not just the brain, but the whole nervous system. Trauma creates patterns of hypervigilance (always bracing for the worst) or hypoarousal (numbness, shutdown). The world can start to feel either too loud or too far away.
And because trauma lives in the body, not just the mind, talk alone isn’t always enough. Regulation requires more than logic. How many times have you said to yourself “Well, LOGICALLY, I know this is what I should do to take care of myself…” It’s not so easy in practice because regulation asks us to engage the body, the senses, and their relationship.
This is something Dr. Gabor Maté explores deeply in The Myth of Normal, where he writes about the ways trauma becomes embedded not just in the brain, but in our physiology, identity, and social patterns. His Compassionate Inquiry approach offers a path toward gently uncovering the roots of stress responses with curiosity instead of shame.
Another impactful read is Stephanie Foo’s *What My Bones Know.* A **powerful memoir that blends personal narrative and journalism to explore the impact of complex PTSD. Her story makes the neuroscience of trauma beautifully human and underscores how much of healing is about being believed, witnessed, and supported.
What Helps: Compassionate Ways to Regulate
So, what can we do?
We begin by understanding that regulation is not about perfection. It’s about returning to a sense of safety, connection, and calm. Some gentle ways to support this:
Breath: Slower exhales activate the parasympathetic nervous system. Try a 4-6 count: inhale for 4, exhale for 6. Check out Dora Kamau’s beautiful meditations on breathwork.
Movement: Walking, stretching, shaking it out — anything rhythmic helps regulate the nervous system.
Co-regulation: Being with someone who feels safe (a friend, therapist, pet) can calm your system faster than anything solo. Polyvagal Theory explains this beautifully.
Sensory grounding: Warm tea, a weighted blanket, music you love. Your senses are the language of safety.
Naming it: Simply saying “I feel overwhelmed” can begin to shift the charge. Also reminding yourself that you are not under threat. Awareness is powerful medicine.
Some other healing-centered voices and tools I recommend:
Deb Dana – Polyvagal-informed practices for safety and connection
Nedra Glover Tawwab – Boundaries and nervous system care
The Nap Ministry – Radical rest as resistance, especially for racialized and marginalized communities
You’re Wired for Survival
If you take one thing from this post, let it be this: your stress responses are not character flaws. They are adaptations — often brilliant, sometimes painful — that helped you survive something hard. Your body remembers what you’ve been through, even when your brain tries to move on.
There is nothing wrong with you. There is something right about a body that tries so hard to keep you safe. With support, with softness, with time, we can teach our brains and bodies what safety feels like again.
Together. Not alone.